Psoriatic Arthritis: Understanding the Connection
Psoriatic arthritis (PsA) is a chronic inflammatory condition that affects both the skin and joints. For individuals with psoriasis, the development of PsA can add another layer of complexity to their health. Understanding PsA, its symptoms, diagnosis, and treatment options is essential for effective management. This article provides a comprehensive overview of psoriatic arthritis and offers insights into living with this condition.
What is Psoriatic Arthritis?
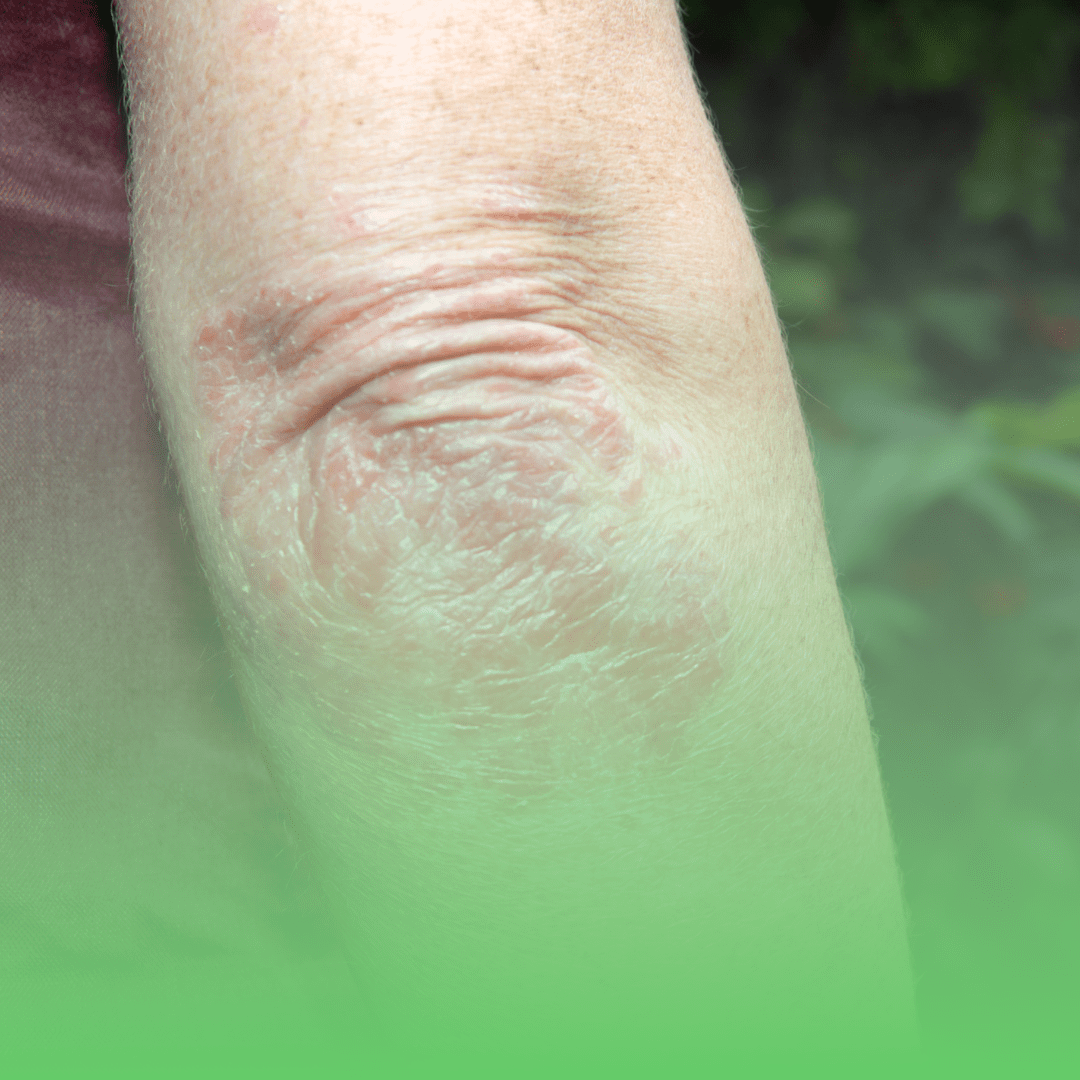
Psoriatic arthritis is an autoimmune disease that causes inflammation in the joints and the places where tendons and ligaments connect to bone. It often occurs in people with psoriasis, a skin condition characterized by red, scaly patches. While psoriasis primarily affects the skin, PsA targets the joints, leading to pain, stiffness, and swelling.
Key Features of Psoriatic Arthritis
- Autoimmune Nature: PsA is an autoimmune disorder, meaning the immune system mistakenly attacks healthy tissue.
- Association with Psoriasis: Approximately 30% of people with psoriasis develop PsA. However, PsA can also occur in people without noticeable skin lesions.
- Joint Involvement: PsA can affect any joint in the body and may involve one or multiple joints.
- Enthesitis: Inflammation where tendons and ligaments attach to bone, a hallmark of PsA, can cause pain and tenderness.
- Dactylitis: Often referred to as “sausage digits,” this involves swelling of an entire finger or toe.
Symptoms and Diagnosis
Recognizing the symptoms of psoriatic arthritis early is crucial for preventing joint damage and managing the condition effectively.
Symptoms
The symptoms of PsA can vary widely among individuals but commonly include:
- Joint Pain and Stiffness: Typically affects the hands, feet, knees, and spine, causing pain and stiffness, especially in the morning or after periods of inactivity.
- Swelling: Joints may become swollen, warm, and tender to the touch.
- Reduced Range of Motion: Joint stiffness can limit movement and flexibility.
- Nail Changes: Pitting, thickening, or separation of the nail from the nail bed, similar to symptoms seen in psoriasis.
- Fatigue: Persistent tiredness and a feeling of being unwell.
Diagnosis
Diagnosing PsA involves a combination of physical examinations, medical history, and diagnostic tests. Early diagnosis is essential to prevent joint damage and manage symptoms effectively.
Physical Examination and Medical History
A thorough physical examination and detailed medical history are the first steps in diagnosing PsA. Your doctor will look for signs of joint inflammation, swelling, and skin lesions indicative of psoriasis.
Imaging Studies
- X-rays: Can help identify joint damage and bone changes associated with PsA.
- MRI and Ultrasound: Provide detailed images of soft tissues, helping detect early joint and tendon involvement.
Laboratory Tests
- Blood Tests: While there is no specific blood test for PsA, tests such as the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) can indicate inflammation. Rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies are usually negative in PsA, helping distinguish it from rheumatoid arthritis.
Treatment Options
There is no cure for psoriatic arthritis, but various treatments can help manage symptoms, reduce inflammation, and prevent joint damage. Treatment plans are individualized based on the severity of symptoms and specific needs.
Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Benefits: Reduce pain and inflammation.
- Side Effects: Gastrointestinal issues, increased risk of cardiovascular problems with long-term use.
- Disease-Modifying Antirheumatic Drugs (DMARDs)
- Benefits: Slow disease progression and prevent joint damage.
- Common DMARDs: Methotrexate, sulfasalazine, and leflunomide.
- Side Effects: Liver damage, bone marrow suppression, lung problems.
- Biologics
- Benefits: Target specific components of the immune system to reduce inflammation and slow disease progression.
- Common Biologics: TNF inhibitors (etanercept, infliximab, adalimumab), IL-17 inhibitors (secukinumab, ixekizumab), and IL-23 inhibitors (ustekinumab, guselkumab).
- Side Effects: Increased risk of infections, injection site reactions.
- Janus Kinase (JAK) Inhibitors
- Benefits: Block specific pathways involved in the inflammatory process.
- Common JAK Inhibitors: Tofacitinib and upadacitinib.
- Side Effects: Increased risk of infections, blood clots, and changes in blood counts.
Physical Therapy and Exercise
Physical therapy can help maintain joint flexibility, reduce pain, and improve overall function. A physical therapist can design an exercise program tailored to your needs, including:
- Range-of-Motion Exercises: To maintain and improve joint flexibility.
- Strengthening Exercises: To support joint stability and overall strength.
- Aerobic Exercise: Activities like walking, swimming, or cycling to improve cardiovascular health and reduce fatigue.
Lifestyle Modifications
Making certain lifestyle changes can significantly impact the management of PsA:
- Healthy Diet: A balanced diet rich in anti-inflammatory foods (fruits, vegetables, whole grains, lean proteins) can help reduce inflammation and improve overall health.
- Weight Management: Maintaining a healthy weight reduces stress on the joints and can alleviate symptoms.
- Stress Management: Techniques such as meditation, yoga, and mindfulness can help manage stress, which can trigger flare-ups.
Surgical Options
In severe cases where joint damage is extensive, surgical options such as joint replacement or repair may be necessary to restore function and relieve pain.
Conclusion
Psoriatic arthritis is a complex condition that requires a comprehensive approach to diagnosis and treatment. Early recognition of symptoms and prompt diagnosis are crucial for effective management. With a combination of medications, physical therapy, lifestyle modifications, and ongoing medical care, individuals with PsA can lead active, fulfilling lives. Always consult with a healthcare provider to develop a personalized treatment plan that addresses your specific needs.
Bibliography
- Gladman, D. D., Antoni, C., Mease, P., Clegg, D. O., & Nash, P. (2005). Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Annals of the Rheumatic Diseases, 64(suppl 2), ii14-ii17.
- Ritchlin, C. T., Colbert, R. A., & Gladman, D. D. (2017). Psoriatic Arthritis. The New England Journal of Medicine, 376(10), 957-970.
- Mease, P. J., & Armstrong, A. W. (2014). Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs, 74(4), 423-441.
- Ogdie, A., & Gelfand, J. M. (2015). Clinical risk factors for the development of psoriatic arthritis among patients with psoriasis: a review of available evidence. Current Rheumatology Reports, 17(10), 64.
Keywords
- Psoriatic arthritis
- PsA
- Psoriasis
- Autoimmune disease
- Joint inflammation
- Enthesitis
- Diagnosis
- Treatment options
- Biologics
- DMARDs
