Understanding Psoriasis: A Guide for New Psoriasis Warriors
Psoriasis is a chronic skin condition that affects millions of people worldwide. If you’ve recently been diagnosed with psoriasis, you might feel overwhelmed and unsure about what lies ahead. As a doctor, I want to provide you with clear, easy-to-understand information about this condition, so you can feel empowered and confident in managing it. Remember, you are not alone; the Psoriasis Warrior community is vast and supportive.
What is Psoriasis?
Psoriasis is an autoimmune disease that primarily affects the skin. In a healthy immune system, your body’s defense mechanisms protect you from infections and illnesses. However, in autoimmune conditions like psoriasis, the immune system mistakenly attacks healthy cells. This abnormal immune response leads to the rapid production of skin cells, causing them to build up on the surface of the skin. The result is thick, red, scaly patches that can appear anywhere on the body.
Types of Psoriasis
There are several types of psoriasis, each with its own unique characteristics:
- Plaque Psoriasis: The most common form, characterized by red, raised patches covered with a silvery-white buildup of dead skin cells.
- Guttate Psoriasis: Appears as small, dot-like lesions and often starts in childhood or young adulthood.
- Inverse Psoriasis: Found in skin folds, such as under the breasts, in the groin, or around the buttocks, and is characterized by bright red, shiny lesions.
- Pustular Psoriasis: Characterized by white pustules (blisters of noninfectious pus) surrounded by red skin.
- Erythrodermic Psoriasis: A severe, very rare type that leads to widespread redness and scaling, covering a large area of the body.
Causes and Triggers
While the exact cause of psoriasis is not fully understood, we know that it involves a combination of genetic, environmental, and immune system factors. Here are some key points:
- Genetics: Psoriasis often runs in families. If a close relative has psoriasis, you may have a higher risk of developing it.
- Immune System: In psoriasis, the immune system speeds up the growth cycle of skin cells.
- Triggers: Certain factors can trigger or worsen psoriasis, including stress, infections, skin injuries, smoking, and specific medications.
Symptoms
Psoriasis symptoms can vary depending on the type and severity. Common symptoms include:
- Red patches of skin covered with thick, silvery scales
- Dry, cracked skin that may bleed
- Itching, burning, or soreness
- Thickened, pitted, or ridged nails
- Swollen and stiff joints (psoriatic arthritis)
Diagnosis
If you suspect you have psoriasis, it’s essential to see a doctor for a proper diagnosis. A dermatologist, a doctor who specializes in skin conditions, can diagnose psoriasis based on the appearance of your skin and medical history. In some cases, a skin biopsy (removing a small sample of skin for examination) may be necessary to confirm the diagnosis and rule out other conditions.
Treatment Options
While there is no cure for psoriasis, many treatments can help manage symptoms and improve your quality of life. Treatment plans are personalized based on the type and severity of psoriasis, as well as individual preferences and lifestyle. Here are some common treatment options:
Topical Treatments
- Corticosteroids: Reduce inflammation and slow down skin cell turnover.
- Vitamin D Analogues: Slow skin cell growth.
- Retinoids: Normalize DNA activity in skin cells.
- Salicylic Acid: Promotes the shedding of dead skin cells.
- Coal Tar: Reduces scaling, itching, and inflammation.
Phototherapy
- UVB Phototherapy: Exposes the skin to ultraviolet B light.
- PUVA: Combines a drug called psoralen with UVA light.
Systemic Treatments
- Oral or Injected Medications: For moderate to severe psoriasis, including biologics that target specific parts of the immune system.
Lifestyle and Home Remedies
- Moisturizing: Regular use of moisturizers to keep the skin hydrated.
- Stress Management: Techniques such as yoga, meditation, and mindfulness.
- Healthy Diet: Incorporating anti-inflammatory foods.
Living with Psoriasis: Tips and Support
Living with psoriasis can be challenging, but with the right strategies and support, you can manage your symptoms effectively and maintain a positive outlook. Here are some tips to help you navigate life as a Psoriasis Warrior:
- Stay Informed: Knowledge is power. Stay informed about your condition and treatment options. The more you know, the better you can manage your psoriasis.
- Follow Your Treatment Plan: Adherence to your treatment plan is crucial. Consistency in using prescribed medications and therapies can make a significant difference.
- Moisturize Regularly: Keep your skin hydrated to prevent dryness and scaling. Use a high-quality, fragrance-free moisturizer.
- Avoid Triggers: Identify and avoid factors that trigger your psoriasis flare-ups, such as certain foods, stress, and skin injuries.
- Practice Stress Management: Stress can worsen psoriasis. Engage in activities that help you relax and manage stress, such as yoga, meditation, or hobbies you enjoy.
- Stay Active: Regular exercise can help reduce stress, improve mood, and maintain a healthy weight, all of which can positively impact your psoriasis.
- Eat a Healthy Diet: A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can help manage inflammation.
- Protect Your Skin: Take care of your skin by avoiding harsh soaps and hot water. Wear sunscreen and protective clothing when outdoors.
- Join Support Groups: Connecting with other Psoriasis Warriors can provide emotional support and practical advice. Look for local or online support groups.
- Communicate with Your Healthcare Team: Keep an open line of communication with your doctor and healthcare team. Regular check-ins can help adjust your treatment plan as needed.
- Be Patient: Managing psoriasis is a long-term journey. Be patient with yourself and recognize that improvement may take time.
- Stay Positive: Maintaining a positive outlook can make a significant difference in your overall well-being. Celebrate small victories and focus on what you can control.
- Educate Others: Raise awareness about psoriasis by educating your friends, family, and community. This can help reduce stigma and promote understanding.
- Get Enough Sleep: Prioritize good sleep hygiene to ensure you get enough rest. Quality sleep is essential for overall health and can help manage stress.
- Avoid Smoking and Alcohol: Both smoking and alcohol can trigger or worsen psoriasis symptoms. Limiting or avoiding these substances can benefit your skin and overall health.
The Power of the Psoriasis Warrior Community
One of the most empowering aspects of living with psoriasis is knowing that you are part of a strong, supportive community. The Psoriasis Warrior community is vast and full of individuals who understand the challenges and triumphs of living with this condition. Connecting with others who share similar experiences can provide emotional support, practical advice, and a sense of belonging.
Conclusion
Being diagnosed with psoriasis can be daunting, but remember that you are not alone. With the right information, treatment, and support, you can manage your symptoms and lead a fulfilling life. Embrace your identity as a Psoriasis Warrior, stay informed, and reach out to the supportive community around you. Together, we can navigate this journey and thrive.
If you have any questions or concerns about your condition or treatment plan, don’t hesitate to contact your healthcare provider. A proper diagnosis and personalized treatment plan are crucial for managing psoriasis effectively.
Stay strong, stay positive, and know that you have the power to take control of your health and well-being.
TYPES OF PSORIASIS
Getting the right diagnosis is crucial in managing psoriasis. At Psodex, we cannot provide a medical advice, but our blog posts are designed to help you better understand your condition.
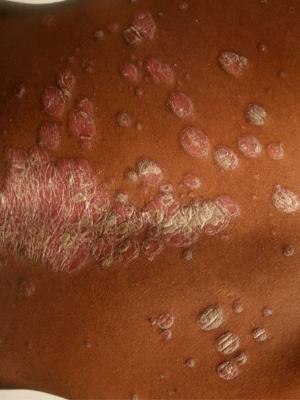
Plaque Psoriasis (Psoriasis Vulgaris)
Characterized by raised, red patches covered with silvery scales; its most distinctive feature is the presence of plaques.
Key Symptoms:
- Plaque-like raised, red patches covered with silvery scales.
- Often appears on elbows, knees, scalp, and lower back.
- Itchy and may cause discomfort or pain.
- Can be associated with nail changes, such as pitting or thickening.

Guttate
Psoriasis
Exhibits small, red, drop-like lesions scattered over the trunk, limbs, and scalp; its most distinctive feature is the scattered nature of its lesions.
Key Symptoms:
- Small, red, drop-like lesions scattered over the trunk, limbs, and scalp.
- Often triggered by bacterial infections, such as strep throat.
- More common in children and young adults.
- Can resolve spontaneously but may develop into chronic plaque psoriasis.

Inverse Psoriasis (Flexural Psoriasis)
Presents smooth, red patches without scales, often in skin folds; its most distinctive feature is its occurrence in skin folds.
Key Symptoms:
- Smooth, red patches without scales, often in skin folds like the armpits, groin, under the breasts, and around the genitals.
- Prone to irritation from friction and sweating.
- May be mistaken for fungal infections due to its appearance.

Pustular
Psoriasis
Manifests as white pustules surrounded by red skin, either localized or generalized; its most distinctive feature is the presence of pustules.
Key Symptoms:
- Can be localized to certain areas of the body or generalized.
- Characterized by white pustules (blisters filled with pus) surrounded by red skin.
- Types include localized, generalized, and palmoplantar pustulosis.
- May be accompanied by fever, chills, itching, and rapid skin scaling.

Erythrodermic Psoriasis
Involves widespread redness and shedding of scales affecting most of the body surface; its most distinctive feature is the extensive skin redness and shedding.
Key Symptoms:
- Rare but severe form characterized by widespread redness and shedding of scales affecting most of the body surface.
- Skin may appear burnt and feel extremely itchy or painful.
- Can cause severe dehydration, infection, and disruptions in body temperature regulation.
- Requires immediate medical attention due to its potential life-threatening complications.

Psoriatic
Arthritis
Causes joint pain, stiffness, and swelling in individuals with psoriasis; its most distinctive feature is the involvement of joints, leading to arthritis symptoms.
Key Symptoms:
Inflammatory joint disease that affects some people with psoriasis.
Symptoms include joint pain, stiffness, swelling, and decreased range of motion.Can affect any joint, including the fingers, toes, spine, and large joints like the knees and hips.
May cause nail changes, such as pitting, thickening, or separation from the nail bed.






